Medical and chiropractic authorities now agree that the treatment of back and/or leg pain from disc herniation by skilled manipulation is proven both safe and effective,1,2 and that disc herniation should now be seen primarily as a non-surgical disease to be treated by conservative methods.3
What is a Disc and why does it ‘slip?’
The anatomy of the human spine includes 24 bones (vertebrae) each separated by a spongy, jelly filled sac, known as an intervertebral disc. Normally, before the age of 30, the discs are very strong and forgiving, and trauma to your spine (poor posture, car accidents, falls, sports etc.) are often perceived as causing no problems as there is little discomfort suffered. However, prolonged wear and tear takes its toll on the disc structure.

An expanded view of the lower lumbar segments.
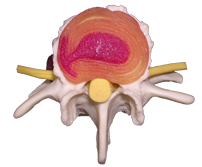
Top view of an intervertebral disc model showing nuclear material extending through a radial tear into a concentric tear and characteristic “anchor sign”. The outer disc fibres are pain sensitive.

Poor core stability and lack of deep abdominal muscle contraction on normal flexion movement. Many movements like this in daily life contribute significantly to disc injury.

MRI scan showing 2 healthy (white) discs and a large disc protrusion (black disc) with nerve compression in a 16 year old girl.

MRI cross section showing the same disc protrusion pushing backwards and completely obliterating the nerve causing severe sciatica.
One of the first changes to take place is deterioration of the disc’s jelly-like centre (the nucleus pulposis). The resilient fluid filled disc becomes dry, replaced by coarse collagen fibres. The ‘drying’ of the disc causes it to become saggy and less supportive.
As the disc sags the cartilage plates of the two vertebrae get closer to each other. This causes the disc to bulge. If this process is allowed to continue further damage occurs.
Normally, the disc acts as a supportive shock absorber for the spine. However, the degenerative changes that occur as a result of the loss of pressure within the disc, promote instability of the spinal joints. The instability allows a greater amount of uncontrolled movement to occur in the joints of the spine. This leads to more thinning and eventually bulging of the disc occurs.
Your body weight is no longer supported by the centre of the disc but instead the walls of the sac (annulus fibrosis.) The thinner and weaker a disc becomes the greater the chance of a disc protrusion gets. This process is commonly referred to as a “slipped disc”. Increased tension on the annulus leads to bony spurs forming on the edges of the vertebrae in an attempt to stabilise the spine.
If the disc is allowed to bulge far enough it will protrude into the space in which the spinal cord and nerves sit. Pressure on the neural tissue, by the disc, results in symptoms ranging from a mild ache to severe sciatic pain. The severity of the symptom is not always a good indication of the state of the disc. Clinically, a very small disc protrusion can cause as much, or more, discomfort as a large protrusion. The mild backache that you experience from time to time may be as a result of a thinning disc or a tearing annulus fibrosis.
It is crucial for people experiencing acute back pain to seek help. It is also very important for those people who have been involved in car accidents or are subjected to other forms of repeated trauma (golf swing, cricket, tennis, etc.) and even those who spend a lot of time sitting at a desk to seek assessment by someone who is professionally trained to assess the function of your spine.
References
- Cassidy, J.D., Thiel, H.W., Kirkaldy-Willis, K.W. (1993) Side posture manipulation for lumbar intervertebral disc herniation. J. Manip. Physiol. Ther. 16: 96-103.
- Nwuga, V.C.B. (1982) Relative therapeutic efficacy of vertebral manipulation and conventional treatment in back pain management. Am. J. Phys. Med. 6: 273-278.
- Bozzao, A., Gallucci, M. et al. (1992) Lumbar disc herniation: MR Imaging assessment of natural history in patients treated without surgery. Neuroradiology. 185: 135-141.
