Everything else you didn’t already know about scoliosis.
It was an honour to be recently asked by Dr. Anthony O’Reilly from The Chiropractic Alumni (tCa) to present a lecture on the “Neurology of Scoliosis” at a Sydney College of Chiropractic and Macquarie University Department of Chiropractic Conference (20 August 2011). The conference, held at the Stamford Grand in North Ryde was solely dedicated to Scoliosis and it was good to be speaking alongside A/Prof. Lindsay Rowe (radiologist and author of Essentials of Skeletal Radiology), Dr. Jeb McAviney (Internationally recognised scoliosis expert) and Dr. Inger Villadsen (European rehabilitation specialist).
What follows is a summary of the latest neurological information on scoliosis and the new relationships being discovered between brain imbalance and scoliosis.
While the lecture was more specifically written for practitioners, I have adapted some of the content to help educate those interested in scoliosis. So, if some of the information is too detailed, just breeze through that section, until it becomes more sensible again. The trouble with neurology is its amazing complexity – but it sure is interesting and understanding it has much to offer those who have scoliosis.
Introduction
Scoliosis is probably the most common spinal deformity encountered in clinical practice. But, if you look up scoliosis in the index of renowned child and adolescent neurology textbooks, and other neurology texts, it is surprising to find nothing under that heading. This is because traditionally, scoliosis is thought of as an orthopaedic condition, more related to bone structure and not neurological control over the musculoskeletal system.
The goal of the following information is to have practitioners and patients appreciate that scoliosis is not only a 3-dimensional deformation of the spinal column, it is a condition of the neuromusculoskeletal system. In fact, it is almost certainly much more related to neurology than biomechanical.
As for the seriousness of scoliosis, it has been associated with a lower quality of life (1-3), lower scores on health questionnaires (4),and a greater likelihood of developing chronic pain more often than the general population (5). The average curvature progression in idiopathic scoliosis is more than 7 degrees per year (6).
From the mechanical viewpoint, most chiropractors, osteopaths and physiotherapists are quite comfortable with the idea that a short leg may contribute to a scoliosis. But is this all there is to it? Is it solely the result of a short leg? Or carrying a schoolbag over the same shoulder? As chiropractor Matthew Long recently said on a blog – it might be time to move on from the idea of schoolbags causing scoliosis – and for good reason.

Recent thoughts on the cause of scoliosis
Many of the proposed etiologies of idiopathic scoliosis are neurological in origin, including brain asymmetry (7), neural axis deformities (8), and central nervous system processing errors (9) and integrative problems (10,11). So, how might poor sensory input from muscles, ligaments and spinal joints to our brain contribute to scoliosis? Remember, that we have 100 billion neurons in our brain and up to 80,000 connections between each neuron. The question is, can a failure in communication between our sensory system, which perceives where we are in space, and our motor system, which coordinates our response to that position in space, be responsible for scoliosis?
Well, our sensory system receives information through our visual, vestibular and proprioceptive systems. Postural and physiological responses to this sensory information then need to be coordinated by our nervous system. Muscles need to be activated so we don’t fall over when we change position, or move our limbs, and blood flow changes are necessitated so there is the correct amount of fuel delivery to the appropriate tissues. So if I pump my right arm, not only does my left brain (cortex) need to give the message for volitional movement, but the correct amount of blood needs to be delivered to oxygenate the biceps and triceps muscles.
Our position in space needs to be attended to by our brain’s structures. Many people, when asked to march on the spot with the eyes closed (Fukudas marching test), find they spin one way or the other. It may indicate a failure of sensorimotor integration pathways and more particularly, is a likely issue with the cerebellum. These sensorimotor deficits don’t have to be so dramatic. Subtle signs, such as a simple head tilt allow suitably trained chiropractors to pick up the possibility of poor cerebellar function.
The true etiology of idiopathic scoliosis remains unknown; however, it appears to be multifactorial (12,13). It was thought for some time that melatonin (a sleep-wake hormone from the pineal gland of the brain) played a role in the development of scoliosis. And this was because in the mid 1990s experiments revealed that the removal of a chickens pineal gland resulted in scoliosis – and administration of melatonin prevented scoliosis in those same chickens (14). Multiple authors have since been unable to identify significant differences in melatonin levels in patients with adolescent idiopathic scoliosis (15,16,17).
In 2005, Cheung and his colleagues found that none of 18 pinealectomised monkeys developed scoliosis within a period of 28 months, strongly suggesting that the possible causative factors producing idiopathic scoliosis in chickens are different from primates (18). Just this year a paper was published showing that on positron emission tomography (PET) there was no significant difference in melatonin secretion and no melatonin deficiency between patients with adolescent idiopathic scoliosis and the control group (13). So, the data regarding human melatonin levels are mixed at best, and the melatonin deficiency as a causative factor in the development of scoliosis is no longer supported.
Scoliosis and the relationship to the brain
Research is now moving towards brain-based models of scoliosis development. The idea that a defective sensory input, or an anomalous sensorimotor integration, may lead to abnormal postural tone and the development of a spine deformity. Domenech and colleagues from the Dept. of Orthopaedic Surgery in Valencia, Spain (19,20) now suggest that
“a deregulation with hemispheric asymmetry in the modulation of the motor activity controlling spine posture at (an) intracortical level could be the cause of progressive scoliotic deformity.”
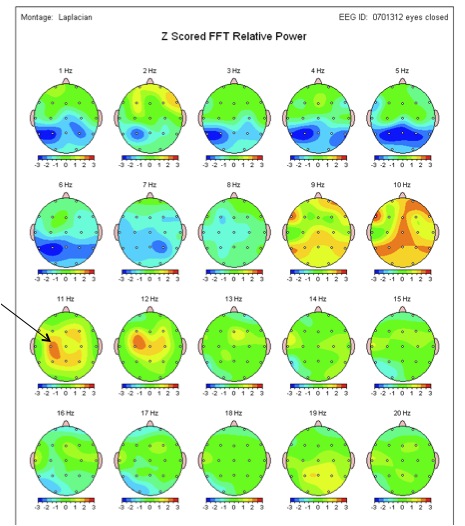
Again, this shows that there is a possible difference in brain activity from one side to the other which may drive what will become asymmetrical motor tone on one side of the body compared to the other. This is certainly supported by unpublished data from Stephen Sexton, chiropractor from Melbourne who utilises QEEG (quantitative electroencephalogram) in practice (a way of measuring electrical brain activity). In this 12 year old girl with a >30 degree scoliosis, Stephen has found an imbalance in 11-12Hz activity on QEEG. This likely indicates there is excessive idling in the brain and certainly indicates hemispheric asymmetry in the sensorimotor areas of the brain overlying the frontal and parietal lobes.
Functional MRI studies have also demonstrated over-activity of secondary motor areas of the cortex (20). It was found that patients with idiopathic scoliosis showed a significant overactivation of the supplementary motor area (SMA) while performing motor tasks as compared to healthy controls. This cortical area has a significant role in posture control.
What is also interesting, is that many coexistent neurological alterations are present in scoliosis patients, such as visual deficiency (21) and decreased postural stability (22,23). So, it seems that scoliosis may be the result of failure to integrate sensory information for cortical processing.
Scoliosis and Primitive Reflexes
Many chiropractors are familiar with retained primitive reflexes and the concept of them being integrated through an organised higher cortex. Our primitive reflexes are controlled by the brainstem and associated lower centres. They are stimulus elicited, and involve automatic and stereotyped movements, respiration, autonomic, and glandular responses without cortical input. These reflexes which we have all possessed are essential for survival and provide an immediate response to environmental needs at a time when higher cortical centres have not yet developed sufficiently. The reflexes anatomically and neurologically stay for the remainder of our life and it is why practitioners may even test adults for the grasp reflex or other signs that the higher cortex is not dampening or inhibiting lower brain reflexes.
Primitive reflexes ideally begin to function in a particular order and are integrated in a specific sequence. For scoliosis they are important in relation to:
- Vestibular integration
- Visual function
- And the development of succeeding primitive and postural reflexes.
As our primitive reflexes are integrated (mostly in the first 6-12 months of life) postural reflexes emerge, so that by 8 months a baby may begin to crawl, sit by itself and then walk from 12-14 months. We have various primitive reflexes – one in particular potentially being related to scoliosis.
Spinal Galant Reflex
The Spinal Galant reflex usually begins about 18 weeks after conception and is normally integrated at 2-4 months, but may persist until 1 year old. It appears to take an active role in the birth process, helping the newborn work its way down the vaginal canal. If one strokes down the low back to one side of the spine in a newborn it will elicit side bend of the lumbar spine and elevation of the hip on the same side. Stimulation down both sides of the spine will activate a related reflex, which causes urination. A retained Spinal Galant reflex often creates the “ants in the pants” school child as the pressure from the chair elicits the reflex and they begin to squirm. Because of the relationship with urination, they will also often have poor bladder control and nocturnal enuresis (night time bed wetting). If unilateral (one-sided), a scoliosis or a limp is possible.

If present, this reflex can be identified by a chiropractor and then addressed so that it may be integrated at a cortical (brain) level as it should have been in those first few months.
Scoliosis and the Visual System
We are learning that patients affected by idiopathic scoliosis show not only a spinal deformity, but also postural and oculomotor deficits. The prevalence of scoliosis in a population of blind women was 42% while the prevalence in the general population in the same region is 3% (13). In another study of 75 children who were visually handicapped and 728 healthy control participants they found 5 times more back surface abnormalities in the blind population (21). This is presumably because you have lost one of the 3 sources of sensory information to the brain (visual, vestibular and proprioceptive) and there is some loss of cortical information with the loss of sight.
Manzoni and Miele have suggested that scoliosis is not simply a vestibular problem but more likely
“a disrupted integration of vestibular and visual signals at the cortical level, (which) may lead to an altered perception of the vertical and to abnormal motor commands.” (24)
In its most severe form, horizontal gaze palsy with progressive scoliosis (HGPPS) is a rare autosomal recessive disorder (25-27) characterised by congenital absence of horizontal gaze, progressive scoliosis, and failure of the motor and sensory tracts to cross within the brainstem. This condition highlights the relationship between our sensorimotor system and the control of our spine.
Idiopathic scoliosis
The term idiopathic is Greek for “pathology unto itself”. But essentially it means that there is no known cause. Idiopathic scoliosis is considered in three age groups:
Infantile
- 0-3 years old
- Nine out of ten of these curves will spontaneously resolve within 6 weeks.
- Left-sided curves are commonly seen, particularly in boys.
- MRI suggested if >20 degrees or if not resolved in 6 weeks.
- More than 20% will have a neural axis abnormality such as Arnold-Chiari malformation, syringomyelia, or cord anomaly on MRI (28).
Juvenile
- 3-9 years old
- May rapidly progress especially in children over the age of five and may require orthotic (brace) management
- ~20% prevalence of neural axis abnormalities in patients if curve is >20 degrees.
Adolescent
- 10-18 years old
- Most common and represents about 80% of idiopathic scoliosis.
- Incidence of very small curves is similar in both sexes.
- Curves in the treatment category are more common in girls than boys (~10:1).

If we look for a moment at adolescent idiopathic scoliosis, girls, for unknown reasons, have a significantly higher risk for development of curve progression than boys. Is it because they have larger brains? While the boys are out hunting, the girls are at home communicating, multi-tasking and developing a larger brain. The female brain and pathways will myelinate faster and develop muscle tone early – on a skeletal system that may not be strong enough (particularly if there is cortical asymmetry and abnormal sensorimotor integration).
Unfortunately, scoliosis awareness seems to have been on the decrease and community nurse assessment of young school children has reduced. We know that school screening is ideally performed in girls in Years 7 and 9 (11 and 13 years of age) and the notification rate should be less than 3%. The Spine Society of Australia recommends Year 7 assessment only if both cannot be afforded but more recently the abandonment of school screening programs has led to the introduction of the National Self-Detection Program for Scoliosis. A brochure should be provided by the school which will place responsibility for curve detection on the adolescent population and parents.
As a general rule, assessment should involve visual inspection and a forward bend test looking for early signs of rib humping. Click here for more information on how to detect a scoliosis.


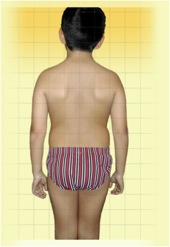
This is a good example of a double curve that was undetected during her growing years. These types of curves are often missed because they seem to cancel each other out when the child or adult is standing. They are often only noticed when the child bends forward as the degree of rotation is maximised. She has a 65-degree lumbar curve and a 75-degree thoracic curve.

Neurological Pathways involved in Scoliosis
Movement and posture is complex and requires much modulatory control, particularly through the reticular system of the brainstem. To control our movement there are 2 major groups of descending motor pathways:
Lateral pathways
Control both proximal and distal muscles and are responsible for most voluntary movements of the limbs.
- Lateral corticospinal tract
- Rubrospinal tract
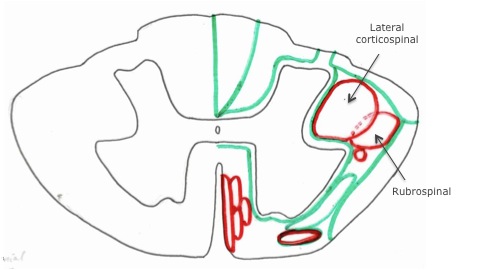
Medial pathways
Responsible for posture, balance and coarse control of axial and proximal muscles.
- Vestibulospinal
- Reticulospinal
- Tectospinal
- Anterior corticospinal
The motor nuclei of the ventral horn in the spinal cord are arranged along a medial-lateral axis according to function (29). The ventromedial motor nucleus innervates axial muscles of the spine – and is supplied by the medial motor pathways. The dorsolateral motor nucleus innervates limb musculature, with more distal muscles of the limb being most lateral – and is supplied by the lateral motor pathways.
The tectospinal and reticulospinal tracts are a major alternate route (to the pyramidal tract) by which spinal motor neurons are controlled. They lie adjacent to the parts of the grey matter that they will influence. For instance, the lateral reticulospinal tract carries fibres that will influence the IML (intermediolateral column) in the thoracic cord, responsible for sympathetic changes to blood supply. The medial reticulospinal tract influences the medial ventral horn, where our axial cells predominate for spinal posture (quite neat how the reticulospinal tract wraps itself around the ventral horn).
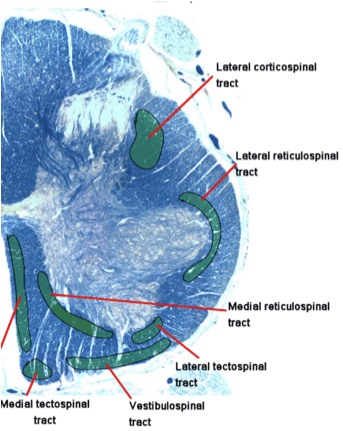
Reticulospinal neurons are capable of initiating motor function. Those who have incomplete spinal cord injury can learn to walk using these “older pathways”. The reticular neurons of the brainstem receive an enormous drive from the cortex on the same side and these reticular neurons of the brainstem contribute to muscle tone via the reticulospinal tract.
So, the medial descending pathways from the brainstem project to the ventromedial motor nucleus of the spinal cord, which contains the cells of the spinal column muscles. The muscles that provide core stabilisation.
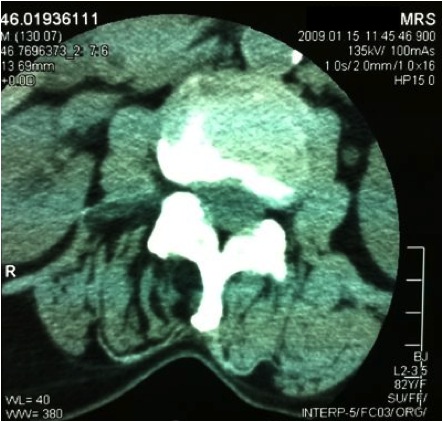
In this example, there is extensive fatty infiltrate (black areas) of the deep spinal (multifidi) muscles on the right side. While this may be argued to be disuse there is good reason to think that it was caused by loss of tone and likely decreased influence from the cortex on the same side through the reticular formation (within the brainstem). More simply, our left brain controls volitional (wanted) movement on our right, but our right brain controls the resting muscle tone – and it does this through the brainstem or reticular formation.
Our eye muscles and spinal muscles work through the same neuronal system and complex integration of pathways. So, if there is a breakdown in eye movements, it is possible there is a breakdown in the coordination of intrinsic spinal muscles. A skilled practitioner can examine their coupled motion during assessment and this will help determine the level of control, not only of the eyes, but of the core stabilising muscles of the spine.
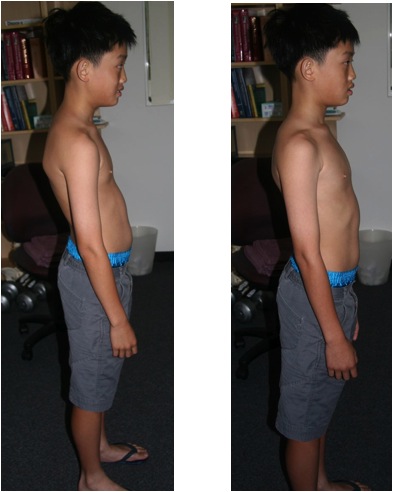
This young boy (8 yo) presented with an inability to read at appropriate school age level, and poor posture. Much more subtle, but he is unable to pursuit a visual target smoothly, indicating a soft (sub-clinical) lesion. This certainly explains why he is unable to read a line in a book. He also has a host of retained primitive reflexes, including the asymmetrical tonic neck reflex (ATNR) and you can see his head turn to the right when he looks to the right. (Sorry, video currently unavailable)
Chiropractic and Scoliosis
The spine is by far the greatest source of proprioceptive input, firing to the midline nuclei of the cerebellum. The intertransverse muscles of the spine have the greatest concentration of muscle spindles compared to any other tissue, closely followed by the suboccipital muscles of the cervical spine. The midline nuclei of the cerebellum fire back down as the vestibulospinal tracts, utilising the vestibular nucleus, to contract the muscles that resist gravity. Our brain relies upon only three needs – oxygen, fuel and activation. If there is prolonged poor input to the cerebellum, such as poor proprioceptive input from dysfunctional spinal joints, there will potentially be poor vestibular output via the cerebellum – resulting in poor muscle tone.
Immediate improvements in posture may be attributed to improvement in descending control of motor neuronal pools. This occurs through improved proprioceptive integration at the cerebellar and cortical level and acting through the vestibulospinal and reticulospinal systems.
Scoliosis treatment is not just about hitting the high spots and trying to push curves back into place. We might have to preference sidedness of an adjustment to selectively target one part of the sensorimotor cortex over another. Appropriate exercises may need to be given to train certain brain pathways to be activated. And regular tailored homecare exercises may contribute to a better outcome.

Our spine stays in line due to the neural integrity that is maintained in our axial system through descending spinal pathways. As chiropractors we can influence this neural integrity and recent studies have shown that manipulation of the spine seems to influence the nervous system at many levels. Research from Heidi Haavik-Taylor shows that cervical spine manipulation changes sensorimotor integration. Using transcranial magnetic stimulation, changes were discovered within the sensorimotor cortex following a single cervical spine manipulation (30). These changes were also seen in patients who had dysfunctional cervical joints (31) and the central nervous system was found to respond differently following cervical manipulation after motor training tasks compared to normals (32).
Scoliosis is not just an orthopaedic condition anymore. It is a condition that affects the nervous system’s control of the muscles on the skeletal system and as such needs to be looked at in this way. It is more likely that scoliosis occurs when sensory information from our visual, vestibular and proprioceptive sources is inappropriately combined at a cortical level, with subsequent over-activation of motor circuits involved in postural control. The change to sensorimotor integration that is offered to some scoliotic patients through chiropractic may just be what is needed.
If, as the research suggests, one of the potential causes of scoliosis is cortical asymmetry, maybe our best defence against an idiopathic scoliosis is a “balanced brain”. Particularly at the age where there is to be a large growth spurt.
For a practitioner who may be able to help you detect or manage scoliosis please call Shirley Rd Chiropractic Crows Nest (02 9966 0992).
This information was written by Brent Gordon from Shirley Rd Chiropractic and as such remains his intellectual property. For practitioner use of this information please contact his offices.
References
1. Shapiro GS, Taira G, Boachie-Adjei O: Results of surgical treatment of adult idiopathic scoliosis with low back pain and spinal stenosis: a study of long-term clinical radiographic outcomes. Spine 2003, 28:358-363.
2. Danielsson AJ, Nachemson AL: Radiologic findings and curve progression 22 years after treatment for adolescent idiopathic scoliosis: comparison of brace and surgical treatment with matching control group of straight individuals. Spine 2001, 26:516-525.
3. Freidel K, Petermann F, Reichel D, Steiner A, Warschburger P, Weiss HR: Quality of life in women with idiopathic scoliosis. Spine 2002, 27:E87-E91.
4. Schwab F, Dubey A, Pagala M, Gamez L, Farcy JP: Adult scoliosis: a health assessment analysis by SF-36. Spine 2003, 28:602-606.
5. Weinstein SL, Dolan LA, Spratt KF, Peterson KK, Spoonamore MJ, Ponseti IV: Health and function of patients with untreated idiopathic scoliosis: a 50-year natural history study. JAMA 2003, 289:559-567.
6. Chuah SL, Kareem BA, Selvakumar K, Oh KS, Borhan Tan A, Harwant S: The natural history of scoliosis: curve progression of untreated curves of different aetiology, with early (mean 2 year) follow up in surgically treated curves. Med J Malaysia 2001, 56(Suppl C):37-40.
7. Niesluchowski W, Dabrowska A, Kedzior K, Zagrajek T: The potential role of brain asymmetry in the development of adolescent idiopathic scoliosis: a hypothesis. J Manipulative Physiol Ther 1999, 22:540-544.25.
8. Dobbs MB, Lenke L, Szymanski DA, Morcuende JA, Weinstein SL, Bridwell KH, Sponseller PD: Prevalence of neural axis abnormalities in patients with infantile idiopathic scoliosis. J Bone Joint Surg Am 2002, 84-A:2230-2234.
9. Lowe TG, Edgar M, Margulies JY, Miller NH, Raso VJ, Reinker KA, Rivard CH: Etiology of idiopathic scoliosis: current trends in research. J Bone Joint Surg Am 2000, 82-A:1157-1168.
10. Chen PQ, Wang JL, Tsuang YH, Liao TL, Huang PI, Hang YS. (1998) The postural stability control and gait pattern of idiopathic scoliosis adolescents. Clin Biomech 13:S52-S58.
11. Lao ML, Chow DH, Guo X, Cheng JC, Holmes AD (2008) Impaired dynamic balance control in adolescents with idiopathic scoliosis and abnormal somatosensory evoked potentials. J. Paed. Orthop. 28:846-9.
12. Lowe TG, Edgar M, Margulies JY, Miller NH, Raso VJ, Reinker KA, Rivard CH. Etiology of idiopathic scoliosis: current trends in research. J Bone Joint Surg Am. (2000) 82:1157-68.
13. Girardo M, Bettini N, Dema E, Cervellati S. (2011) The role of melatonin in the pathogenesis of adolescent idiopathic scoliosis (AIS). Eur Spine J. 20:S68-74. Department of Spine Surgery, Turin, Italy.
14. Machida M, Dubousset J, Imamura Y, Iwaya T, Yamada T, Kimura J. (1995) Role of melatonin deficiency in the development of scoliosis in pinealectomised chickens. J Bone Joint Surg Br.77(1):134-8.
15. Hilibrand AS, Blackmore LC, Loder RT, Greenfield ML, Farley FA, Hensinger RN, Hariharan M. (1996) The role of melatonin in the pathogenesis of adolescent idiopathic scoliosis. Spine 21:1140-6.
16. Fagan AB, Kennaway DJ, Oakley AP. (2009) Pinealectomy in the chicken: a good model of scoliosis? Eur Spine J. 18: 1154-9.
17. Brodner W, Krepler P, Nicolakis M, Langer M, Kaider A, Lack W. (2000) Melatonin and adolescent idiopathic scoliosis. J Bone Joint Surg Br. 82: 399-403.
18. Cheung KM, Wang T, Poon AM, Carl A, Tranmer B, Hu Y, Luk KD, Leong JC. (2005) The effect of pinealectomy on scoliosis development in young nonhuman primates. Spine 15: 2009-13.
19. Domenech J, Tormos JM, Barrios C, Pascual-Leone A (2010) Motor cortical hyperexcitability in idiopathic scoliosis: could focal dystonia be a subclinical etiological factor? Eur Spine J. 19:223-30
20. Domenech J, Garcia-Marti G, Marti-Bonmati L, Barrios C, Tormos JM, Pascual-Leone A. (2011) Abnormal activation of the motor cortical network in idiopathic scoliosis demonstrated by functional MRI. Eur Spine J. 20:1069-78.
21.Catanzariti JF, Salomez E, Bruandet JM, Thevenon A: Deformity, Visual Deficiency and Scoliosis. Spine 2001, 26:48-52.
22.Nault ML, Allard P, Hinse S, Le Blanc R, Caron O, Labelle H, Sadeghi H: Relations between standing stability and body posture parameters in adolescent idiopathic scoliosis. Spine 2002, 27:1911-1917.
23.Chen PQ, Wang JL, Tsuang YH, Liao TL, Huang PI, Hang YS: The postural stability control and gait pattern of idiopathic scoliosis adolescents. Clin Biomech 1998, 13(Suppl 1):S52-S58.
24. Manzoni D and Miele F. (2002) Vestibular mechanisms involved in idiopathic scoliosis. Arch Ital Biol. 140:67-80.
25. W-M Chan, E I Traboulsi, B Arthur, N Friedman, C Andrews, E C Engle (2006) Horizontal gaze palsy with progressive scoliosis can result from compound heterozygous mutations in ROBO3. J Med Genet 2006;43:e11. USA
26. Bosley TM, Salih MA, Jen JC, Lin DD, Oystreck D, Abu-Amero KK, MacDonald DB, al Zayed Z, al Dhalaan H, Kansu T, Stigsby B, Baloh RW. (2005) Neurologic features of horizontal gaze palsy and progressive scoliosis with mutations in ROBO3. Neurology 12;64:1196-203.
27. Jen JC. (2008) Effects of failure of development of crossing brainstem pathways on ocular motor control. Prog Brain Res 171:137-41.
28. Dobbs MB, Lenke LG, Szymanski DA, Morcuende JA, Weinstein SL, Bridwell KH, Sponseller PD. (2002) Prevalence of neural axis abnormalities in patients with infantile idiopathic scoliosis. J Bone Joint Surg Am. 84:2230-4.
29. Kandel ER, Schwartz JH, Jessell TM (2000) Principles of Neural Science, 4th ed. McGraw-Hill, New York.
30.Taylor HH and Murphy B. (2008) Altered sensorimotor integration with cervical spine manipulation. JMPT 31:115-126.
31. Taylor HH and Murphy B. (2010) Altered central integration of dual somatosensory input after cervical spine manipulation. JMPT 33:178-188.
32. Taylor HH


Thanks for this post. It helps so much.. I am very happy to see this type of blog.